My butterfly effect is turning into a birth story healer after my own traumatic birth.
I used to get this question all the time: “Why do you want to have such a niche? Isn’t it enough if the person who gave birth and the baby are okay?” It angers me to no end when folks say unintentionally hurtful things like “at least you are okay” when folks share that they had a traumatic birth. This minimizes the key role the transition into parenthood has on becoming parents. It’s one thing to be okay after such a transformative and life-changing event. I strive to be better than okay.
The week that falls around July 15 is dedicated to raising awareness about birth trauma and its effects on families. As a therapist who supports people with this type of trauma, initiatives that honour birth trauma are important to me. As a mother who had a traumatic first birth, this week is even more important – I feel validated and seen.
I am honoured to support new parents to heal from this form of trauma. And yes, not all people who give birth identify as mothers, and the non-birthing parent can experience trauma from the birth too. As a trauma therapist, trained in various ways to process trauma, i knew that this would be a way to offer support and be in the best service.
Let me backup a bit and share what trauma is, so that we are on the same page, literally and figuratively. Here is a shorter and more concise, if not a bit simple summative definition: Trauma is something that happens too fast, too much or is too big so it impacts a person‘s experience. It causes overwhelm and can have a lasting toll. It can also be something that takes too long, is experienced alone, and there is not enough information or support. It also shows up as not enough care, not enough time, or not enough support. It’s both extremes because it’s also about being left alone in our experience.
It is not just what happens but also the absence of what should have happened if trauma didn’t get in the way. This is why all trauma has a felt sense of grief. Further, someone can continue to have unresolved trauma because they didn’t have someone witness them in their experience, either immediately or soon after. In short, trauma happens when something is too overwhelming for someone, and they feel alone in the experience.
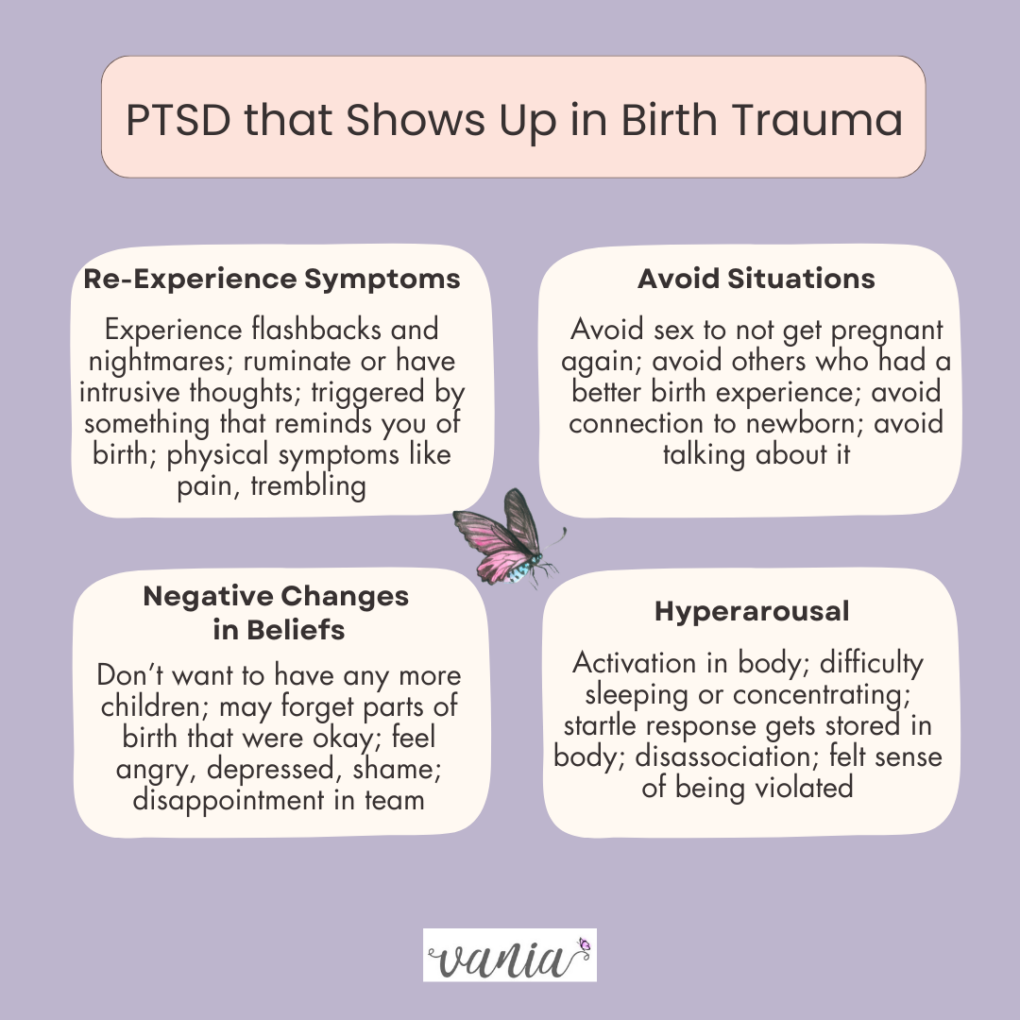
 This is also why a birth that does not go according to plan, and in fact can be quite dysregulating, can also be seen as a trauma. It is the experience of something that’s overwhelming, as well as the absence of what you wanted to happen. It has emotional and psychological impacts because of the distressing childbirth experience. The emotional toll of birth trauma is vast, and can lead to a diagnosis of Post-Traumatic Stress Disorder (PTSD). Birth Trauma is different from perinatal mood challenges, and yet the symptoms are similar. So, it needs to be given the same attention and care. Like all traumas, it is up to the person who experienced it, not professionals or anyone else – it is truly in the eye of the beholder (Thanks to Cheryl Beck for this reference.)
This is also why a birth that does not go according to plan, and in fact can be quite dysregulating, can also be seen as a trauma. It is the experience of something that’s overwhelming, as well as the absence of what you wanted to happen. It has emotional and psychological impacts because of the distressing childbirth experience. The emotional toll of birth trauma is vast, and can lead to a diagnosis of Post-Traumatic Stress Disorder (PTSD). Birth Trauma is different from perinatal mood challenges, and yet the symptoms are similar. So, it needs to be given the same attention and care. Like all traumas, it is up to the person who experienced it, not professionals or anyone else – it is truly in the eye of the beholder (Thanks to Cheryl Beck for this reference.)
One in 3 birthers experience birth trauma and that number is even higher for racialized mothers, people with disabilities, queer and gender diverse parents. This number has also increased to closer to 45% of all births during the pandemic.
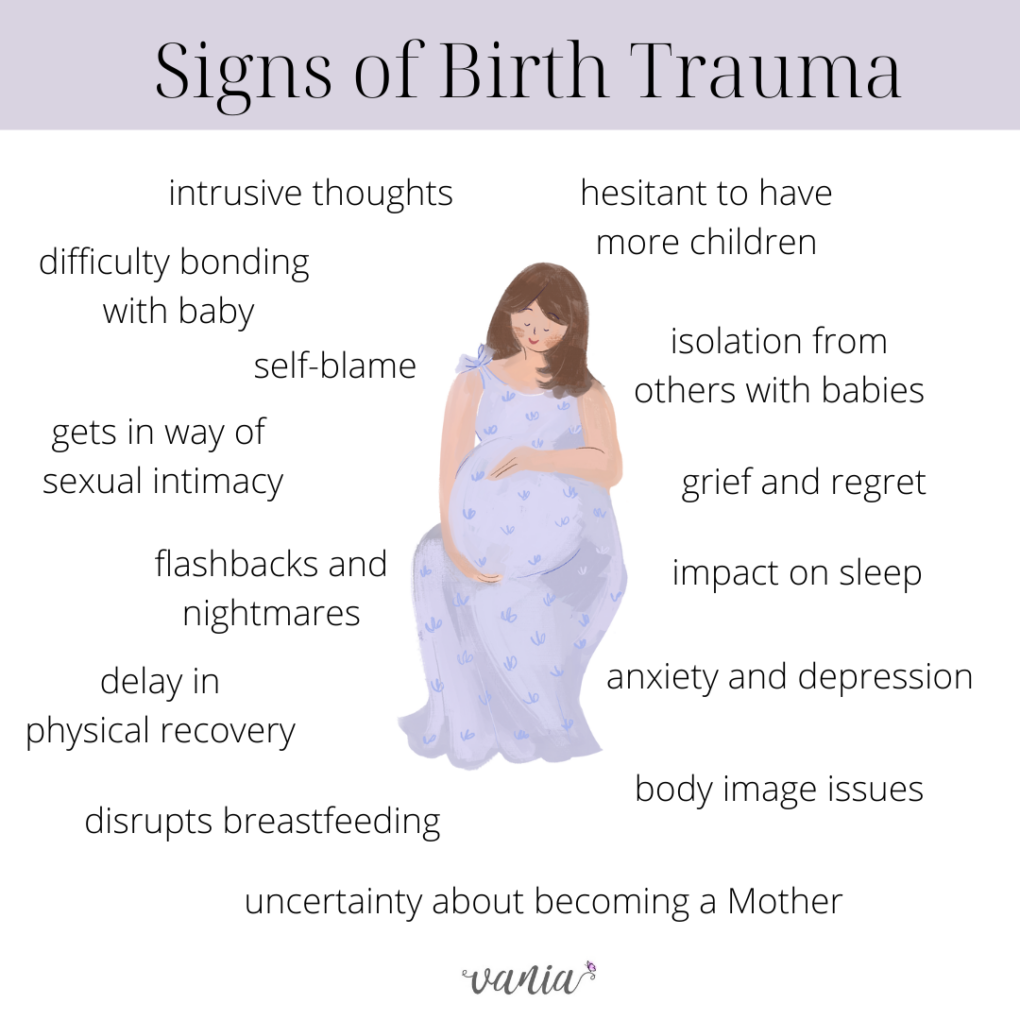
To paint this picture, i’m going to share some hard facts about the impact of birth trauma. You may want to be mindful of your needs as you read this.
It’s helpful to know there are more than 1 kind of traumatic birth, in fact there are several distinct types of Birth Trauma: 1) Objective Experiences like the death of the newborn or the birther or serious injury to birther or newborn; 2) Subjective Experiences like a fear of own life or of newborns; 3) Systemic Failure and Obstetric Violence that makes the birther feel not heard or supported; and 4) Previous trauma that causes re-traumatization. If you want to get a better since of how this impacts people, this article shares one person’s experience after her birth trauma.
This Birth Trauma Tree visual is a powerful depiction of what birth trauma looks like, and how it can impact new parents. Like any experience of trauma, it is up to the person who experienced it to name it as such. Well-intentioned but still hurtful comments may come from family and friends. It’s important to remember that our society has minimized rituals and rites of passage in general, and even more so for rites that are related to “mothering” and women’s labour – literally. It’s no wonder that the focus becomes just about the physical act and not the spiritual metamorphosis as well.
Long-Lasting Complexities of Birth Trauma Show Up:
When others minimize your birth story because ‘everyone is okay’
When your child triggers you now
When it’s not the day you wanted and were told to have
When you blame yourself for the way the birth happened
When your sexual intimacy and body image is impacted
When the birthday of your baby is hard to celebrate
When your plan for having more kids is impacted
When you don’t know that there is support to process it
When you feel like your birth story is not as significant as others who had it worse
 Becoming a parent is a major Rite of Passage in someone’s life. It is a type of initiatory experience. When birth trauma impacts it, the transition is harder and Integration into this new stage of life as a parent can be made more challenging. All rites of passage take time, and are in stages – Separation (i.e. no longer a Maiden); Transition and then Integration of this new role into your full. If you want to listen to a fabulous podcast episode about this, Jessie Harrold interviews Lucy Jones and they talk all about it HERE.
Becoming a parent is a major Rite of Passage in someone’s life. It is a type of initiatory experience. When birth trauma impacts it, the transition is harder and Integration into this new stage of life as a parent can be made more challenging. All rites of passage take time, and are in stages – Separation (i.e. no longer a Maiden); Transition and then Integration of this new role into your full. If you want to listen to a fabulous podcast episode about this, Jessie Harrold interviews Lucy Jones and they talk all about it HERE.
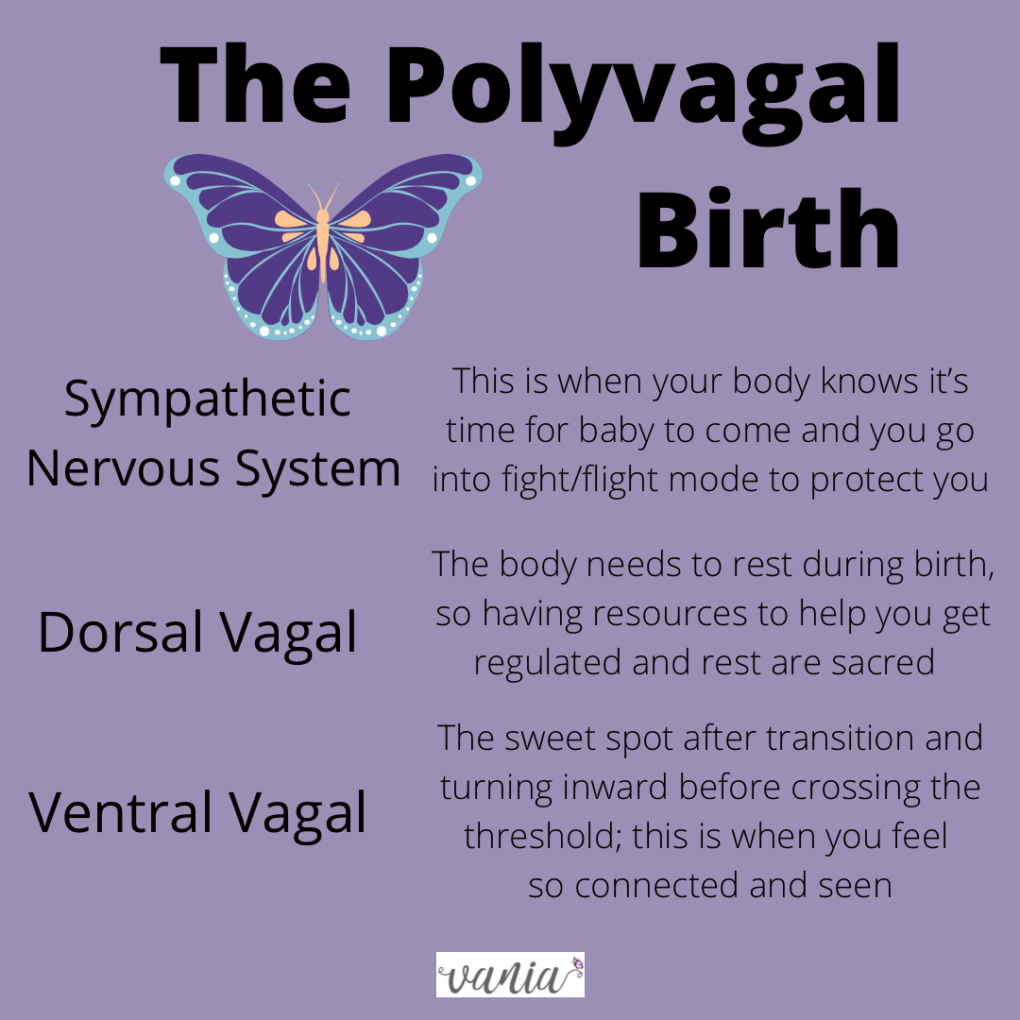
If pregnancy is the cocoon stage of a person’s journey into becoming a parent, birth is seen as the Transition Stage of becoming a parent.The transition to parenthood, and especially motherhood, should be a celebratory and supported time for new parents. This messy transition is not different from any type of sacrifice that is connected to a heroine’s journey. This one is that of becoming something that we have never been before – a mother, a parent. We are entirely new: This is what Matrescence is, the complete physical and spiritual process of becoming someone new, and in this case, a newborn parent (however you birth this child into being). So when the path is altered due to birth trauma, we experience a possible ‘psychotic state’ because we had to do it alone and not be witnessed in it. That is why new parent groups and circles are important and processing birth trauma is key.
 Healing can Happen
Healing can Happen
As i mentioned above, i know that healing can happen because the traumatic birth i experienced with my first-born child was my butterfly effect: it created a ripple effect that changed the trajectory of my life, especially my career. As my initiation into motherhood was rocky, i learned more about birth including it as a rite of passage, the identity crisis, the mood changes, and also that birth can be traumatic. I then made the leap to change the course of my work and specialize in supporting others who had traumatic births.
It was my sliding doors moment, a way to reclaim this transition stage and ultimately experience Post-Traumatic Growth. Trauma healing moves through a spiral-like process, in stages that are paced and intentional. If you are someone who experienced a traumatic birth, it is never too late to receive support and healing. There is a healing quality to being witnessed and having an alternate ending, no matter how long ago you experienced the wound. Here are just some of the resources that i have found helpful:
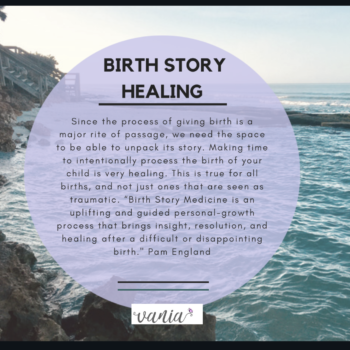
1) Birth Story Processing is one of several therapeutic resources that can help you heal from a traumatic birth. Since as a supportive, narrative re-telling of the story, it can be quite cathartic. I have been trained in Birth Story Medicine with Pam England and have found this process a foundational part of my own healing and how i hold space for others.
2) Kimberly Ann Johnson has a lovely free meditation you can access. It supports your healing and offers healing through self-compassion.
3) Grief Work – need to grieve the birth we wanted so that we can move on. As Francis Weller shares in his powerful book, The Wild Edge of Sorrow, this can be a Gate into grief. It also is a testament of the Hero’s (or Heroine’s) journey. Grief needs to be witnessed and processed, just like birth stories.
4) As trauma is stored in the body, we need to heal the body first. It’s not enough to revisit the story of the birth. We need to reprocess the impact of it on our body. That’s why therapy modalities have incorporated somatic work as a main tenet of care. I have a process to help people unpack and transform their birth story. You can read more about it here. Other helpful resources are EMDR and Somatic Experiencing.
5) One of the Pillars of Post-traumatic Growth is Advocacy. While not a requirement to heal, when we turn what happened to us as a butterfly effect, or sliding doors moment, it is an opportunity for growth and contributing to our community. It helps us shift from our personal experience to a more global common humanity. If you want to read more about how birth trauma can lead to post-traumatic growth, this article (a PDF) does a great job outlining it. Teela has a very informative Instagram account called The Tea on Birth Trauma Here are just some organizations that do this work: Birthtalk and Birth Better.
Of course we want to not need the awareness campaigns and don’t want anyone to experience birth trauma in the first place. For now, we write articles like this and share resources to help you know that healing is possible. You are not alone. We deserve better.
We are not Maidens any longer.



 It’s Time! Baby is on Route
It’s Time! Baby is on Route

 I have mixed feelings about clubs. I never was a Girl Scout, in choir or on sports teams as a kid. I was a dancer though, but that doesn’t seem like the same kind of club or group like the others. For one thing, the rules and homogeneity that seemed to go along with it felt too forced. And just because one kid likes to play soccer, that doesn’t mean she likes the same music or food as another. And it felt like we had to be the same all the time, like Stepford Wives. I could be wrong though.
I have mixed feelings about clubs. I never was a Girl Scout, in choir or on sports teams as a kid. I was a dancer though, but that doesn’t seem like the same kind of club or group like the others. For one thing, the rules and homogeneity that seemed to go along with it felt too forced. And just because one kid likes to play soccer, that doesn’t mean she likes the same music or food as another. And it felt like we had to be the same all the time, like Stepford Wives. I could be wrong though.  Here’s why our well-intentioned comments about someone else’s experience can be problematic: it doesn’t take into account their potential birth trauma and how it’s linked to consent and body trust issues. We hear about birth trauma that relates to obviously upsetting experiences of injury or even infant death. But another type of birth trauma is one where the birther has their voice taken from them, and instead the medical expert is calling all the shots. When some of us have experienced sexual violence and later in life get pregnant, this new experience can bring up former body memories and triggers.
Here’s why our well-intentioned comments about someone else’s experience can be problematic: it doesn’t take into account their potential birth trauma and how it’s linked to consent and body trust issues. We hear about birth trauma that relates to obviously upsetting experiences of injury or even infant death. But another type of birth trauma is one where the birther has their voice taken from them, and instead the medical expert is calling all the shots. When some of us have experienced sexual violence and later in life get pregnant, this new experience can bring up former body memories and triggers.  My eldest child was born 8 years ago this week. Looking back on the birth, i credit the experience i had personally with what motivated me to do the work i do. It wasn’t the birth i wanted, and while i have moments of it that i treasure to this day, parts of it were really scary and it’s taking me time to heal from them. I know i’m one of the lucky ones and my birth trauma is my own story. I also know that i have more tools on hand to heal and delve into the trauma than most of us have. Please read on only if you want to.
My eldest child was born 8 years ago this week. Looking back on the birth, i credit the experience i had personally with what motivated me to do the work i do. It wasn’t the birth i wanted, and while i have moments of it that i treasure to this day, parts of it were really scary and it’s taking me time to heal from them. I know i’m one of the lucky ones and my birth trauma is my own story. I also know that i have more tools on hand to heal and delve into the trauma than most of us have. Please read on only if you want to.  Between 5AM and 11AM my care had to be transferred over to an OB doc. This was devastation #1. I so admired my team of midwives and felt so connected to them, having to be transferred felt like a betrayal even though my Wise Mind knew it was necessary. The doc did not have the same bedside manner or a trauma-informed framework. Ironically, it was the anesthesiologist that helped me get through the discussion that i ‘needed’ to have an emergency C-section. I remember being told that my son’s head was stuck and i was too swollen to give birth vaginally. I remember thinking that in his excitement to meet me, my baby turned a bit too much and got stuck. I remember the pain before the epidural and thinking ‘there is no way that those of us that birth can do this.’ The pain was surreal.
Between 5AM and 11AM my care had to be transferred over to an OB doc. This was devastation #1. I so admired my team of midwives and felt so connected to them, having to be transferred felt like a betrayal even though my Wise Mind knew it was necessary. The doc did not have the same bedside manner or a trauma-informed framework. Ironically, it was the anesthesiologist that helped me get through the discussion that i ‘needed’ to have an emergency C-section. I remember being told that my son’s head was stuck and i was too swollen to give birth vaginally. I remember thinking that in his excitement to meet me, my baby turned a bit too much and got stuck. I remember the pain before the epidural and thinking ‘there is no way that those of us that birth can do this.’ The pain was surreal.  My baby was born that Sunday afternoon, just as the Pride parade was starting. We saw a rainbow out of our minuscule window. It overlooked the lake and i worked hard to rid the delivery/surgery room from my mind. My baby and i worked hard on our latch, our breastfeeding, our bonding. We worked on our rest and healing. We stayed at the hospital for 3 days. We stayed together in our small shared room. We saw other families come in and out. I worked on getting to the bathroom. Devastation #7 is learning the incredible feat of getting out of bed to walk across the room to pee. Devastation #8 is being told i had to work on a poo before leaving the hospital. Yikes, how was that supposed to happen. Devastation #9 is being told that my baby wasn’t latching so wasn’t getting what he needed – i have had my period and big boobs since the age of 9, if nothing else my body was born to breastfeed! He had one dose of formula to get us through that night shift with that 1 nurse. And then i worked my butt off to get him to latch.
My baby was born that Sunday afternoon, just as the Pride parade was starting. We saw a rainbow out of our minuscule window. It overlooked the lake and i worked hard to rid the delivery/surgery room from my mind. My baby and i worked hard on our latch, our breastfeeding, our bonding. We worked on our rest and healing. We stayed at the hospital for 3 days. We stayed together in our small shared room. We saw other families come in and out. I worked on getting to the bathroom. Devastation #7 is learning the incredible feat of getting out of bed to walk across the room to pee. Devastation #8 is being told i had to work on a poo before leaving the hospital. Yikes, how was that supposed to happen. Devastation #9 is being told that my baby wasn’t latching so wasn’t getting what he needed – i have had my period and big boobs since the age of 9, if nothing else my body was born to breastfeed! He had one dose of formula to get us through that night shift with that 1 nurse. And then i worked my butt off to get him to latch.